The Evidence-Informed Decision Making (EIDM) Casebook Issue 2
This issue was published in 2018 and includes nine stories from Canadian public health professionals that demonstrate the use of evidence-informed decision making (EIDM) in a wide range of public health activities, either using evidence to inform a program or intervention, or building capacity for EIDM. The stories describe the initiatives, implementation, evaluation, and lessons learned from using evidence in practice, or building capacity for EIDM.
Download PDF version.
Click here to explore the other issues of the EIDM Casebook.
Access slides and recordings from presentations in the NCCMT’s Peer-to-peer webinar series, featuring authors of stories from the second issue of the EIDM Casebook.
Featured Stories
Allison Branston, Nicole Andruszkiewicz, Cassie Ogunniyi, Dr. M. Mustafa Hirji
Niagara Region Public Health & Emergency Services
To improve the sharing of local demographic and health outcome data to meet the needs of local priority populations, a project was undertaken to examine how to select, analyze and distribute data. Read more about how this team worked to improve data sharing across local public health units and community partners.
Robert Mancini
Health Canada
To help improve the delivery of food safety training, an alternative food safety training model informed by adult learning principles was developed. Read more about the development and implementation of an innovative food safety training course.
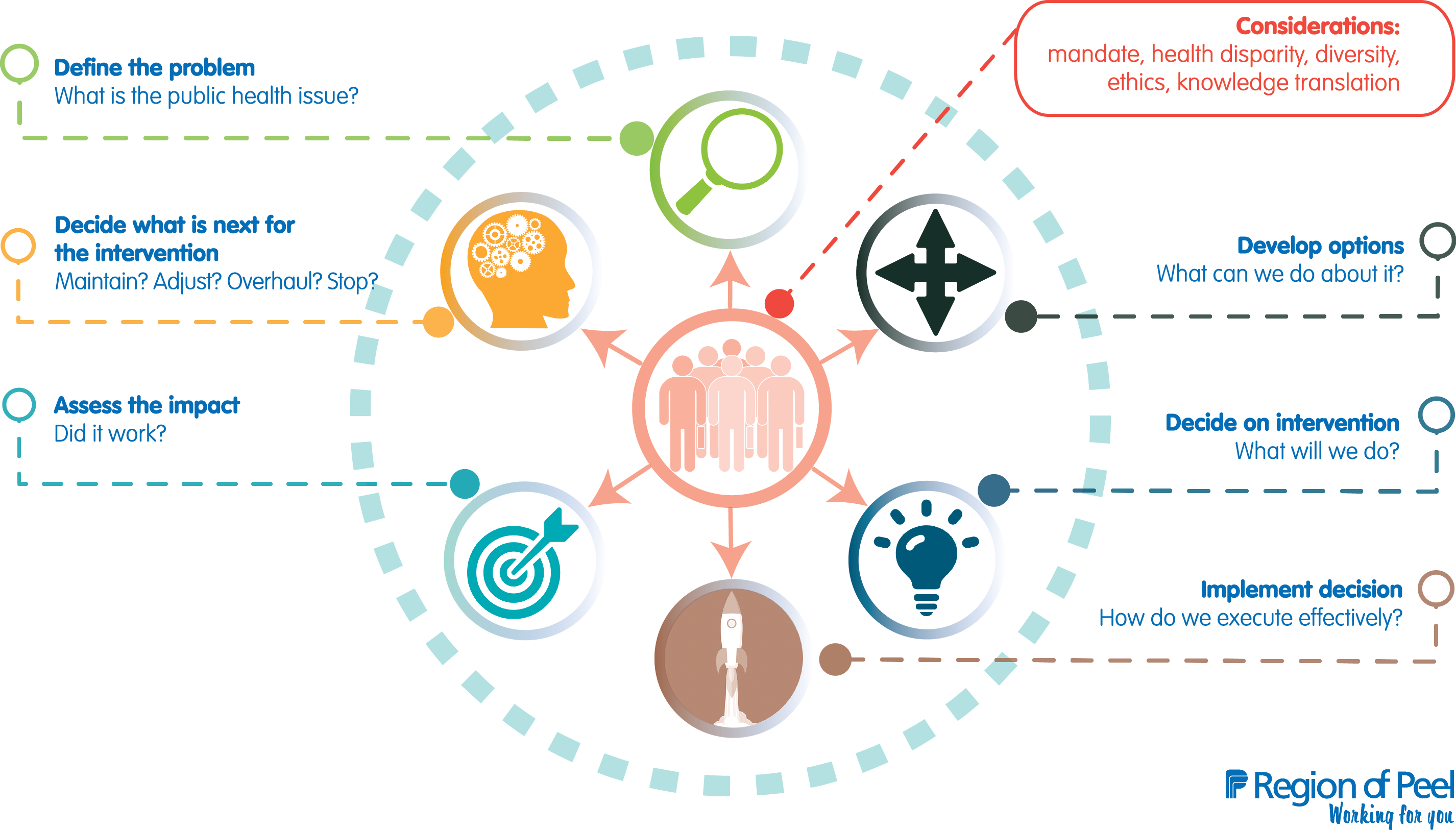
Lori Greco, Dr. Megan Ward
Region of Peel Public Health
Region of Peel Public Health has identified evidence-informed decision making as a strategic priority, termed End-to-End Public Health Practice. Read more about how this health unit is building internal capacity for knowledge brokering and evidence-informed decision making.
Dr. Stephen Bornstein, Rochelle Baker, Pablo Navarro, Sarah Mackey, Aimee Letto, Michelle Ryan
Newfoundland & Labrador Centre for Applied Health Research
The Newfoundland & Labrador Centre for Applied Health Research (NLCAHR) supports applied health research in Newfoundland and Labrador. Read more about how the NLCAHR’s Contextualized Health Research Synthesis Program works with health system partners to prioritize health research needs, as well as synthesize and contextualize evidence for Newfoundland and Labrador.
Ebele Mogo,1 Keiko Shikako-Thomas,1 Annette Majnemer,1 Jonathan Lai,1 Sheila Kennedy,2 Vivien Symington,3 Kellie Duckworth2
1McGill University, 2Sunny Hill Health Centre for Children, 3Club Aviva Recreation
To improve policies on physical activity promotion for people with disabilities, this team undertook a project to bridge the evidence to policy gap. Read more about how a community forum and policy dialogue were used to help bridge this gap and inform policymakers about evidence.
Kristin Beaton
Huron County Health Unit
In an effort to build evaluation and evidence-informed decision making capacity, Huron County Health Unit has implemented several strategies to encourage evaluative thinking. Read more about how this health unit built a learning organizational culture.
J. Cyne Johnston, Farah Bandali, Maureen Devolin, Scarlett Ngoka, Dolly Bondarianzadeh
Alberta Health Services
In Alberta, there was decreasing time available for non-immunization well-child clinic visit activities and these activities varied at clinics across the province. Read more about how these authors used evidence-informed decision making to decide on which routine activities to include in non-immunization well-child clinic activities.
Sana Fakih,1 Jennifer McConnell-Nzunga,1, 2 Jennifer Scarr,1 PJ Naylor,2 Kristin McIlhenney,3 Alex Wilson,4 Vanessa Morley,5 Chris Wright,4 Nicole Fetterly5
1Child Health BC, 2University of Victoria, 3YMCA of Greater Vancouver, 4Sport for Life, 5Childhood Obesity Foundation
Addressing the issue of food and physical literacy, a team from British Columbia developed a strategy to support and promote healthy eating and physical activity in the early years. Read more about how this strategy was designed and implemented.
Dr. Shelina Babul (Co-PI),1 Dr. Ian Pike (Co-PI),1 Dr. Amanda Black,2 Dr. Sarah Richmond,3 Kate Turcotte,1 Samantha Bruin1
1BC Injury Research and Prevention Unit; BC Children’s Hospital; University of British Columbia, 2University of Calgary, 3Public Health Ontario
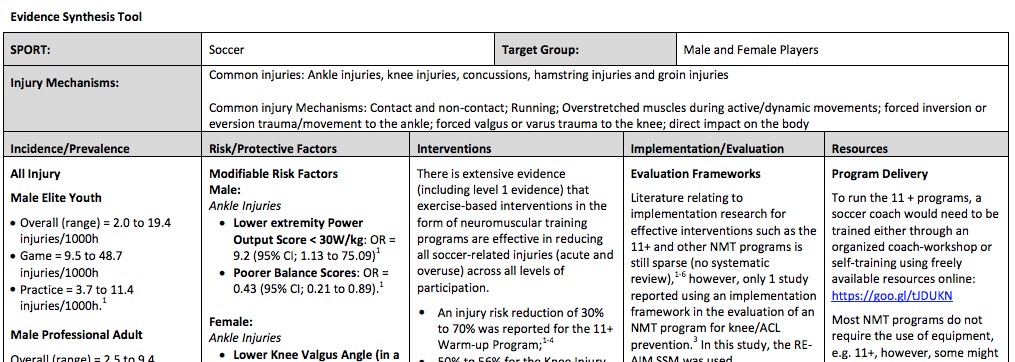
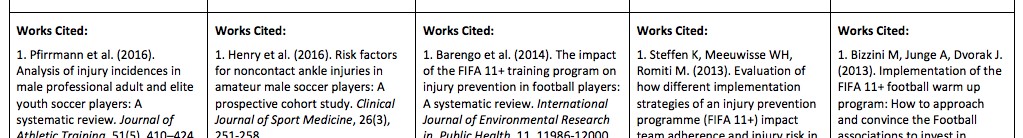
In order to promote evidence-based interventions, a group at the BC Injury Research and Prevention Unit created the website Active & Safe Central. Read more about the development, dissemination and evaluation of this resource.
Full Text Stories
Sharing health information with community organizations to promote health equity
Allison Branston, Nicole Andruszkiewicz, Cassie Ogunniyi, Dr. M. Mustafa Hirji
Niagara Region Public Health & Emergency Services
We would like to acknowledge our team for their contributions to the project:
Andrew Hendriks, BScN, MPH, Ottawa Public Health
Clare Mak, BScN, Kingston, Frontenac and Lennox & Addington Public Health Unit
Elaine Murkin, MSc, Leeds, Grenville and Lanark District Health Unit
Ellen Woodchis, MHSc, MEd, Niagara Region Public Health & Emergency Services
Kaelan Moat, PhD, McMaster Health Forum
Karen Graham, MScN, North Bay Parry Sound District Health Unit
Marty Mako, MBA, Niagara Region Public Health & Emergency Services
Matthew Tenenbaum, MPH, MD, McMaster University
Tina Leung, BScN, MPH, York Region Public Health
Shailee Tanna, MSc, Niagara Region Public Health & Emergency Services
Sinéad McElhone, PhD, Niagara Region Public Health & Emergency Services
Background and Rationale
Local public health agencies (LPHAs) collect local demographic and health outcome data to help identify opportunities to advance health equity work in our communities. Collaboration between LPHAs and community partners (e.g., YMCA, Children’s Services and nonprofits) to share and use this data can help meet the needs of local priority populations. Through consultations prior to this project, Niagara Region community partners identified difficulties related to public health data sharing including limited coordination, use and dissemination of data from public health.
"... Niagara Region community partners identified difficulties related to public health data sharing including limited coordination, use and dissemination of data from public health."
A proposal was submitted to Public Health Ontario (PHO) and funding was approved for a locally driven collaborative project (LDCP) involving six LPHAs from across Ontario. The main objective was to identify ways to best select and analyze key behavioural and health outcome data and how to distribute the data to local community partners.
Objectives
The short-term goals included the following:
- Understand community partners’ preferred types of data and methods of distribution.
- Identify barriers, possible solutions and implementation considerations in data sharing and use among community partners.
- Determine ways in which community partners could use population health data provided to them by LPHAs.
The long-term goals included the following:
- Enable community partners to successfully reduce health inequities.
- Increase data sharing initiatives between LPHAs and their local community partners.
- Develop community partners’ understanding of the role of public health for data sharing.
- Increase understanding among LPHA staff of the data needs of their community partners.
Initiative and Implementation
Phase One
An online survey was conducted to explore the current data usage and needs of community partners across six LPHAs in Ontario. The survey was distributed via individualized emails to 401 community partners with 99 completed surveys returned (25% response rate). The team conducted a literature review in consultation with a librarian to identify how data can be most effectively distributed to community agencies. Inclusion criteria consisted of: literature published between 2007 and the present; publications related to public health data sharing with community stakeholders; literature published in English; and both primary and secondary literature. Databases searched included MEDLINE, EMBASE, and Cumulative Index to Nursing and Allied Health Library (CINAHL). Other sources searched included Google Scholar and grey literature sources. A total of 17 articles were produced after screening titles and abstracts for relevance, of which 12 were deemed relevant after full-text reviews. Two project team members independently critically appraised these articles using the Mixed Methods Appraisal Tool developed at McGill University. Any disagreements in the quality assessments were resolved by consensus.
The findings from the survey and literature review were synthesized into an evidence brief. A deliberative dialogue was conducted in September 2017 to explore how applicable the findings in the evidence brief were to community partners. The discussion included a selection of 16 community partners from various organizations (e.g., homeless shelters, school boards, YMCA) across Ontario that indicated an interest in participating. A dialogue summary was developed to synthesize the information included in the evidence brief along with the discussion from the deliberative dialogue. This dialogue summary described participants’ interest in taking steps toward a common way to collect and share data between LPHAs and community partners. Suggestions included developing data sharing networks, advocating for open-data sharing initiatives and moving toward a universal way to collect social determinants of health (SDOH) data as described in the Tri-Hospital + Toronto Public Health Equity Data Collection Research Project Report.
Phase Two
Phase two included a data sharing pilot that was informed by phase one findings. For this pilot the researchers recruited three community partners from the Niagara Region that were involved in their local community: a primary care service provider, a community-based agency that provides a variety of social services and a local unit of a national agency that provides local services connections. An epidemiologist from Niagara Region Public Health selected data relevant to health equity based on consultations conducted with each of the community partners. Data packages were tailored to the specific needs and interests of each of the three community organizations. The data were aggregated and analyzed without personal identifiers and the results shared with community partners.
Initial evaluations of the pilot found that it was well received by all three community partners. The partners agreed the data were useful for:
- identifying clients they may not be reaching;
- evaluating their services to determine why these audiences are not being reached; and
- demonstrating a need for additional funding/services to address these needs.
The final component of the project was summarizing project findings in a guide that could be used by other LPHAs to facilitate health equity data sharing with their own community partners.

Evaluation and Impact
A one-year impact assessment for this LDCP is currently underway. The main objectives of the impact assessment include the following:
1) To evaluate how data provided to community partners in the pilot may affect their work on health equity related issues. Measurements will include how frequently the data have been used for organizational processes such as funding proposals and re-orientation of existing programs and how the data informed decision-making.
2) To evaluate how the guide can assist LPHAs with sharing data with their local community partners. This will include surveying the guide’s end-users and using web-based metrics to determine the number of times the guide is accessed online.
These objectives will help determine if the project goal of enabling better health equity through data sharing processes with community partners was achieved. A revised version of the guide will be made available on the PHO website by April 2019.
Lessons Learned
What worked well:
- consulting with community partners to build trust and gain an understanding of their data needs
- hosting a deliberative dialogue with community partners to gain an understanding of the barriers and facilitators they face related to data sharing
- having a diverse LDCP team from across Ontario contribute to planning the project, developing evaluation tools and connecting with a range of community partners
Things that could have been done differently:
- consulting with other LHPAs to ensure the guide meets their needs to encourage high uptake of the guide
- increasing the one-year time frame, which limited the time available for team members to review and contribute to project materials
- engaging in a longer pilot with community partners across the province to see how the data sharing relationship develops over time
Back to Top.
An innovative approach to food safety training for temporary and retail operations
Robert Mancini, MSc., CIPHI(C), Environmental Health Officer
Health Canada
Background and Rationale
Food safety training is an integral component in the public health system designed to prevent the incidence of foodborne outbreaks. However, there is a lack of evidence that food safety training programs directly result in improved food hygiene. The majority of food safety courses are delivered in classroom settings or online with no practical component. To assess student knowledge, a written examination is often required to obtain certification. This training is inadequate as it reflects poor training designs that focus only on producing certified personnel rather than paying attention to achieving competency in food hygiene practice.1,2 Food safety training leads to an improvement in food safety only if the knowledge imparted results in a positive change in behavior.3
One key principle of adult learning is that information retention is directly influenced by the amount of practice provided during the learning process.4,5 However traditional food safety training courses are not delivered in this fashion. Providing knowledge to change food safety attitudes and behaviours has not been adequately proven in the literature.3 An effective food training course should not only provide food safety information, it should also implement knowledge into practice for proper retention. Rennie (1994) suggests that training programs that are more closely associated with the work site, coupled with practical reinforcement of hygiene messages, are more effective than traditional methods of training.6 Practical in-house, hands-on activities tend to be the most effective approach in training,7,8,9 although more research is still needed to confirm this.
"An effective food training course should not only provide food safety information, it should also implement knowledge into practice for proper retention."
Objective
The goal of this initiative was to provide an alternative model to the traditional format of food safety training. The hands-on program was initially developed for temporary food service events in Manitoba, and in particular to address comprehension concerns with English as Second Language (ESL) learners. The program was later modified and piloted for Target Corporation, a large food retailer in the United States. Both implementation processes are described below.
Implementation
Temporary Food Service Event (Winnipeg, Manitoba)
The food operator and event coordinator for each pavilion at a temporary food service event participated in two hours of hands-on food safety training. The training covered all facets of food preparation and food service practices, including but not limited to the following:
- How to use a metal stem probe thermometer to test internal food temperatures, including ice bath calibration. A food safety poster depicting safe food internal temperatures was left on-site for ease of reference.
- How to prepare a chlorine-based sanitizer at 100 ppm for effective sanitation. A laminated sticker displaying the colour comparator for strength concentration was given to the operator for reference. The sticker was designed so it could be adhered to a bucket or spray bottle.
- How to perform utensil and pot washing using the three-compartment-sink method.
A commercial kitchen was used as the venue for the hands-on training. The kitchen was divided into eight food safety stations.
|
Food Safety Stations
|
|
Station 1
|
Personnel practices
|
|
Station 2
|
Handwashing
|
|
Station 3
|
Three-compartment sink method
|
|
Station 4
|
Temperature control part 1
|
|
Station 5
|
Refrigerator organization, allergens
|
|
Station 6
|
Temperature control part 2
|
|
Station 7
|
Cleaning and sanitation
|
|
Station 8
|
Record keeping
|
A total of 92 ESL students participated in the hands-on food safety training. In an attempt to accommodate all participants, two separate sessions were offered, each with a class size of 46 participants. The participants were divided into small groups and each group began at a different station. All stations were staffed by a certified public health inspector and/or a food safety specialist who facilitated the activities. The groups rotated through the stations every 15 to 20 minutes. The time at each station was strategically kept short and entertaining to keep participants engaged.
Each station was equipped with a flip chart to assist the facilitator in conducting the training. The charts consisted of compelling pictures, stories and real-life case studies. A number of behavioural science techniques were employed in the training to ensure participant engagement and understanding of the presented materials. Such techniques included the use of storytelling, sharing real-life stories of foodborne illness, using neural encoding (rhymes) and incorporating the principles of consistency and commitment as a means to improve food safety behaviours.
At the end of the training, each participating pavilion was given a food safety package that included the resources necessary to ensure food safety, such as chemical sanitizer test strips, chlorine and quaternary ammonia, hair nets, log sheets and thermolabel test strips. Each participant was given a certificate of participation and was asked to complete an evaluation form for feedback; no exam was administered. The comments on the evaluation forms were overwhelmingly positive and encouraging, and recommended that the program be adopted and administered every year thereafter.
Target Corporation Pilot Hands-on Food Safety Training (Pasadena, California)
The hands-on food safety program was piloted for Target Corporation to determine its effectiveness for a large-scale food retail operation. Pasadena, California was chosen as the site for the pilot due to its high numbers of ESL students.
The implementation of the food safety training program was similar to the temporary food service event scenario, however a classroom was used as the training venue for logistical purposes instead of a commercial kitchen. Further, the participants were granted a recognized food safety certificate, valid for five years, upon successfully passing an exam. The exam was administered through the National Registry of Food Safety Professionals headquartered in Orlando, Florida. A food safety guide, a folder consisting of short and concise food safety reference information, was also distributed to the participants.
The room was divided into six food safety stations and participants rotated through the stations (20–25 minutes) as they engaged in hands-on activities.
|
Food Safety Stations
|
|
Station 1
|
Hazards, cross-contamination
|
|
Station 2
|
Handwashing, personal practices, microbiology
|
|
Station 3
|
Temperature control 1, temperature control 2
|
|
Station 4
|
Cleaning and sanitizing
|
|
Station 5
|
Logs and pests, receiving
|
|
Station 6
|
Equipment and Jeopardy game
|
Two food safety experts facilitated the training. Since the purpose of this training was to certify the participants, a PowerPoint presentation (2 hours) was also delivered for information that could not be communicated via hands-on instruction. The group of 34 participants was divided in half; while half of the participants engaged in the hands-on component, the other half were taught via PowerPoint. After two hours, the groups switched. The PowerPoint presentation incorporated pictures, videos and stories in an effort to make it more compelling.
The pass rate for the class was 94%, significantly higher than any previous year’s pass rate using the traditional food safety training that was strictly classroom-based. Participant evaluations were overwhelmingly positive.
Lessons Learned
The hands-on food safety training program was a success, however logistically a large class size (>20 participants) made implementation of the training more complex and difficult. In such cases, two trainers are necessary to facilitate the hands-on activities, which some jurisdictions may not have adequate resources for. Further, participants were required to take a multiple choice exam to obtain food safety certification, which is typically not psychometrically designed. It is the author’s opinion that a performance test would be a more appropriate method for assessing knowledge of the presented material.
References
1 De Boeck, E., Jacxsens, L., & Vlerick, P. (N.D.). Human behavior and corporate culture may have impact on hygiene, food safety. [ONLINE]. Available at: https://www.news-medical.net/news/20180607/Human-behavior-and-corporate-culture-may-have-impact-on-hygiene-food-safety.aspx (accessed June 2018).
2 Ehiri, J.E., Morris, G.P., & McEwen, J. (1997). Evaluation of a food hygiene training course in Scotland. Journal of Food Control, 8(3), 137-147.
3 Seaman, P. & Eves, A. (2006). The management of food safety—the role of food hygiene training in the UK service sector. Hospitality Management, 25, 278-296.
4 Brabeck, M., & Jeffrey, J. (N.D.). Practice for Knowledge Acquisition (Not drill and kill). [ONLINE]. Available at: http://www.apa.org/education/k12/practice-acquisition.aspx (accessed June 2018).
5 Lieb, S. (1999). Principles of adult learning. [ONLINE]. Available at: http://www.hcc.hawaii.edu/intrnet/committees/FacDevCom/guidebk/teachtip/adults-2.htm (accessed June 2018).
6 Rennie, D. (1994). Evaluation of food hygiene education. British Food Journal, 96, 20-25.
7 Burke, M.J., Sarpy, S.A., Smith-Crowe, K., Chan-Serafin, S., Salvador, R.O., & Islam, G. (2006). Relative effectiveness of worker safety and health training methods. American Journal of Public Health, 96(2), 315-324.
8 Roberts, K.R., Barrett, B.B., Howells, A.D., Shanklin, C.W, Pilling, V.K., & Brannon, L. (2008). Food safety training and foodservice employees’ knowledge and behavior. Food Protection Trends, 28, 252-260.
9 Hendry, C., Jones, A., & Arthur, M. (1992). Skill supply, training and development in the small-medium enterprise. International Small Business Journal, 10, 68-72.
Back to Top.
Knowledge broker training for evidence-informed decision making: Building capacity in public health
Region of Peel Public Health
Background and Rationale
At Peel Public Health, evidence-informed decision making (EIDM) is one component of a 10-year strategic priority known as End-to-End Public Health Practice. EIDM involves the application of research to practice using robust methods for finding, appraising and synthesizing evidence.
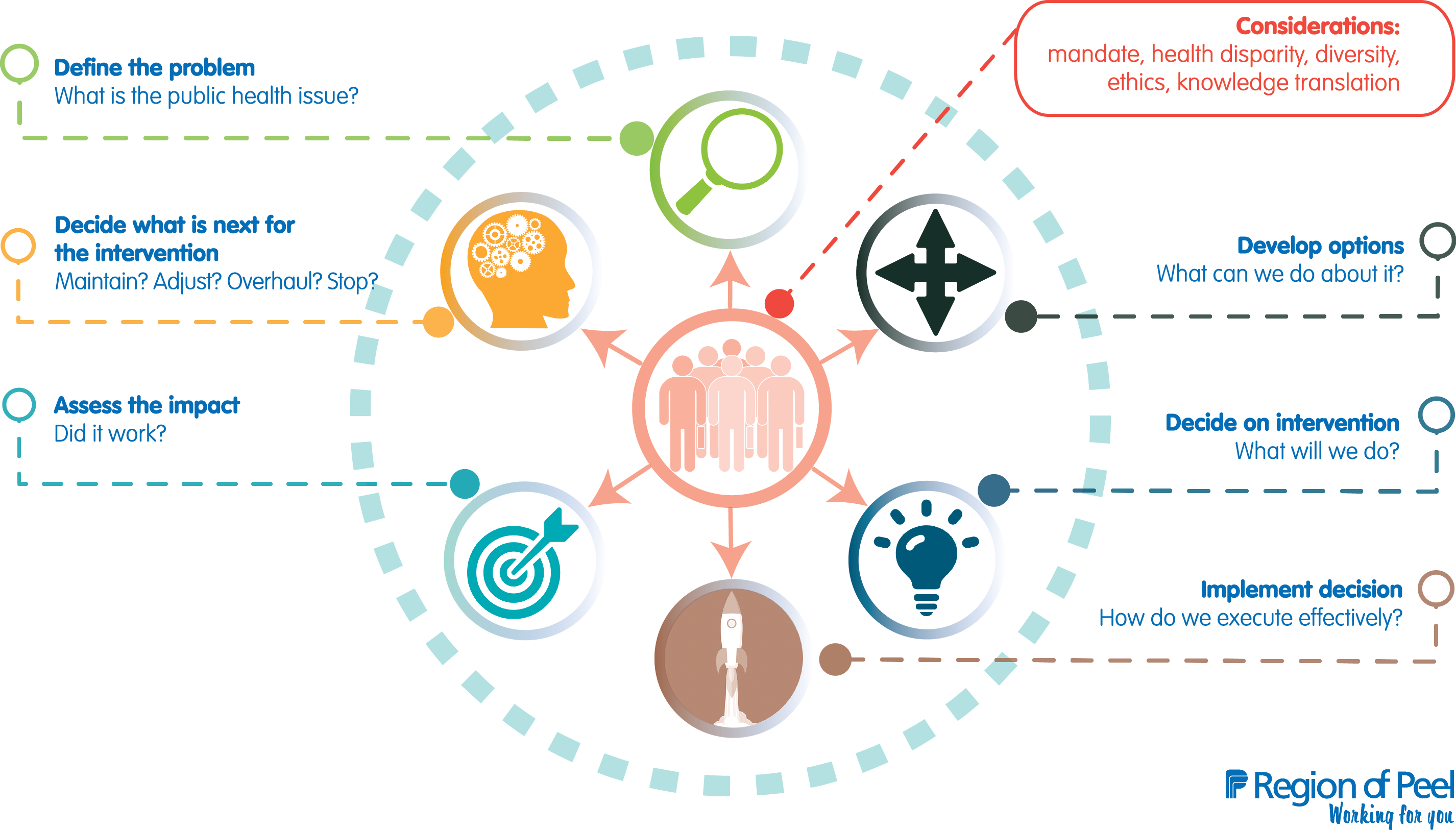
Capacity building for EIDM to date (2009–2018) has included:
- completing an EXTRA (Executive Training Program) project in 2009 to develop processes and tools for research reviews;
- participating in a knowledge broker (KB) case study in partnership with McMaster University in 2009–2011;
- training, including over 130 managers and analysts at the McMaster University week-long EIDM course, two waves of KB training from 2014 to 2018 and tailored training for managers, supervisors and analysts;
- implementing one central and six topic-specific monthly critical appraisal clubs;
- creating a senior KB position in 2014; and
- completing over 75 mentored research reviews.
Expanding the number of KBs through an in-house training program was used to build capacity for EIDM.
Objective
The goal was to have at least one KB in each of five divisions, including Chronic Disease and Injury Prevention, Communicable Disease, Family Health, Health Protection and the Office of the Medical Officer of Health. The objective was to train a cadre of research and policy analysts to become knowledge brokers.
Initiative
Two waves of training programs took place over four years. Analysts in each division were identified by their directors to become knowledge brokers. Analysts were identified based on ability, experience with research reviews, role, interest and career timing.
The training content was based on an in-house literature review identifying KB skills and activities in the following practice areas:
- Research review
- Develop expertise in defining a question; searching for, retrieving, quality assessing and interpreting results; and synthesizing research evidence.
- Mentoring research reviews
- Provide guidance and technical support to teams conducting research reviews.
- Facilitation
- Facilitate dialogue, collaboration and relationship-building to build capacity to find and use research in program decisions (e.g., leading critical appraisal clubs).
- Communication
- Engage with all staff, develop knowledge products and support knowledge sharing among clients.
- Adapt style and content of both verbal and written communication for senior decision-makers, analysts and front-line staff.
- Synthesize and summarize research in a variety of formats, including full reports and one-page summaries.
- Networking
- Become a known resource for EIDM.
- Participating in a KB network to support ongoing learning and collaboration.
Implementation
The senior KB and an associate medical officer of health (AMOH) led the training.
Methods were developed based on adult learning principles, including goal setting, self-direction, focus on current skill and experience, using real-world work for assignments and collaboration. The methods and training structure evolved over two waves of training. Seven analysts started the training in wave one, and wave two included five analysts. All divisions were represented. Each of the analysts devoted one-and-a-half days per week to the training. Each training program took place over two years; the first wave took place over 22 months and the second occurred over 15 months.
Methods for the training included a combination of meetings, practice and mentorship. All training observations, practice, assignments and research reviews were based on real-world work and practice decisions that were taking place in the organization at the time. More specifically, learning strategies included the following:
- reading assigned literature on knowledge brokering
- completing a KB self-assessment and developing a learning contract
- completing tailored projects related to knowledge brokering
- observing the senior KB facilitating various steps in the EIDM process (e.g., critical appraisal meetings) and mentoring analyst/manager teams through research reviews
- practising (as above), followed by one-on-one feedback sessions with the KB
- co-mentoring all research review processes along with the KB
- attending regular group meetings with the AMOH, the KB and other trainees
- conducting ongoing evaluation of progress against learning objectives
Evaluation and Impact
Evaluation of each wave of training consisted of document review; interviews with KB trainees to assess change in knowledge, skill and experience; interviews with their managers to assess change in practice; and reflection by the AMOH and senior KB to assess organizational impact and training methods. Evaluation took place midway and at the end of the training for each cohort.
The evaluation found that intensive, one-on-one mentoring facilitated learning and skill development. Trainees developed leadership, networking, facilitation and research review skills. The evaluation also found that a training team that combined the skills of an experienced KB with the practical knowledge of a senior leader (AMOH) was important for the success of the program.
This type of training takes time. The time investment included approximately three hours per week for the AMOH, 14 hours per week for the senior KB and one-and-a-half days per week for the trainees over the training period. Because trainees worked with supervisors and analysts undertaking research reviews, they had to adjust to real-world schedules. The trainees’ managers needed to commit to the training and readjust work flow as needed. Though not directly involved in training delivery, managers met regularly with trainees to evaluate their progress.
"This type of training takes time. The time investment included approximately three hours per week for the AMOH, 14 hours per week for the senior KB and one-and-a-half days per week for the trainees over the training period."
Learning strategies that included goal setting, observation, practice and feedback appeared to be most effective.
Lessons Learned
- Ongoing support from the entire leadership team ensured organizational commitment over the length of the training.
- Committing sufficient resources and time is essential.
- Focusing on the needs of the clients (i.e., the team conducting the research review) being supported in research review and then starting where they are is necessary and valuable to shepherd staff successfully through research reviews.
- Developing a critical mass of skilled knowledge brokers increases capacity to use research and leads to culture change. We estimate the minimum critical mass is one senior KB plus at least one KB for each division, or approximately one KB per 150 staff.
- Training knowledge brokers results in high quality, robust research reviews that are used to influence practice decisions. Managers feel more confident in decisions when there are high-quality reviews behind them.
- Carefully evaluating the first round of training improved the content and delivery of the training for the second wave.
- Developing advanced skills to use research also improves critical thinking skills and positions knowledge brokers for future leadership roles. Some movement within these roles should be expected (e.g., KBs moving into management positions), resulting in an ongoing need to either recruit skilled KBs or provide subsequent training waves.
References
Bornbaum, C.C., et al. (2015). Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: a systematic review and thematic analysis. Implementation Science, 10, 162.
Dobbins, M., Robeson, P., Ciliska, D., Hanna, S., Cameron, R., O'Mara, L., DeCorby, K., & Mercer, S. (2009). A description of a knowledge broker role implemented as part of a randomized controlled trial evaluating three knowledge translation strategies. Implement Science, 4(1), 23.
Dogherty, E.J., Harrison, M.B., & Graham, I.D. (2010). Facilitation as a role and process in achieving evidence-based practice in nursing: a focused review of concept and meaning. Worldviews on Evidence-Based Nursing, 7(2), 76-89.
Dogherty, E.J., Harrison, M.B., Baker, C., & Graham, I.D. (2012). Following a natural experiment of guideline adaptation and early implementation: a mixed methods study of facilitation. Implementation Science, 7, 9.
Harvey, G., Loftus-Hills, A., Rycroft-Malone, J., Titchen, A., Kitson, A., McCormack, B., & Seers, K. (2002). Getting evidence into practice: the role and function of facilitation. Journal of Advanced Nursing, 37(6), 577-588.
Ward, V., House, A., & Hamer, S. (2009). Knowledge brokering: the missing link in the evidence to action chain? Evidence and Policy, 5, 267-279.
Back to Top.
Putting research in place: An innovative approach to decision support in Newfoundland and Labrador
Dr. Stephen Bornstein, Rochelle Baker, Pablo Navarro, Sarah Mackey, Aimee Letto, Michelle Ryan
Newfoundland & Labrador Centre for Applied Health Research
Background and Rationale
To meet Newfoundland and Labrador’s (NL) mounting healthcare challenges, the province’s health system requires evidence that can be translated into action. Meeting this demand poses its own challenges, including how to prioritize research; how to synthesize an ever-increasing body of complex evidence; how to attune findings to local resources/capacities; and how to produce rapid, easy-to-use reports.
The Contextualized Health Research Synthesis Program (CHRSP) was developed at the Newfoundland and Labrador Centre for Applied Health Research (NLCAHR) to address these challenges. CHRSP provides timely reports on priority topics by involving health system partners at every stage, from topic identification to uptake. Taking a further step, CHRSP attunes its research to the unique characteristics of the NL healthcare context, including an aging (largely rural) population, a high burden of chronic disease, a demand for better mental health services, the challenges of serving a small population dispersed over a large geography, human health resource challenges and mounting fiscal pressure to do more with less. By considering such contextual factors, CHRSP has achieved considerable uptake for its reports among target stakeholders: provincial health system leaders, senior administrators and other key health system decision-makers.
Objectives
CHRSP was established to provide decision support for improved health services delivery in the province. Its goals include the following:
- Identify health system priorities.
- Include health system partners as research participants.
- Critically appraise and apply an evidence rating system for included studies, emphasizing systematic reviews.
- Synthesize high-quality evidence.
- Produce reports quickly in flexible formats: Evidence in Context reports (10 months, 30–50 pages, 4-page summary, and briefing note); Rapid Evidence reports (30 days, 10–15 page summary) and Snapshot reports (40-day jurisdictional scans).
- Contextualize findings for NL.
- Promote mutual learning—researchers learn about health system realities and system partners learn about research and its applications.
Initiative
Key components of CHRSP include:
- partnerships with deputy ministers from two government departments (Health & Community Services and Children, Seniors & Social Development) and the CEOs of four regional health authorities and their delegates (CHRSP Champions);
- health system involvement from issue identification to dissemination;
- a focus on local context in framing the research and reporting findings;
- economical use of resources and staff;
- a combination of local expertise and subject-matter experts from outside the province; and
- rapid turnaround by focusing on systematic reviews and recent primary studies.
Our approach involves seven steps:
1. Topic Selection: CHRSP consults annually with deputy ministers from two government departments and CEOs from four regional health authorities to identify upcoming decisions that could benefit from research input. CHRSP champions (senior decision-makers) within each stakeholder organization link CHRSP to health system workers/leaders to develop a roster of topics.
2. Prioritization: Once topics have been submitted from across the healthcare system for potential CHRSP study, the CHRSP team collaborates with the CHRSP champions, the health authority CEOs and the deputy ministers to prioritize these topics, giving executives the opportunity to compare their challenges with those faced by their provincial colleagues. The CEOs and deputy ministers then take a final vote to derive an annual consensus list of topics. By participating in this priority-setting process, CHRSP researchers gain valuable insight into the strategic priorities and policy concerns of the provincial healthcare system.
3. Team Building: CHRSP contracts a national/international subject expert to lead a project team that includes the following:
- a health system leader (deputy minister, CEO, delegate)
- a health economist (when required)
- CHRSP program director, project coordinator and researchers
- health system and academic co-investigators and context advisors
- member(s) of a Patient/Caregiver Advisory Council
4. Evidence Gathering/Synthesis/Assessment: CHRSP searches for evidence from systematic reviews, meta-analyses, health technology assessments, high-quality primary studies published too recently for inclusion in the review literature and grey literature. Systematic reviews are assessed for quality using AMSTAR (Assessment of Multiple Systematic Reviews) and primary studies are assessed using the Downs & Black checklist.
CHRSP has also developed its own automated Evidence Rating System (ERS) to compute the strength of the evidence for each intervention/outcome combination abstracted from the selected reviews and studies. For each combination, the ERS assesses three factors—the methodological quality of the studies used, the number of unique primary studies synthesized by the reviews and the degree of consistency of the evidence—to rate the evidence for each intervention/outcome combination on a five-point scale (very strong, strong, moderate, weak or very weak). The ERS is conservative by design, discounting any findings deemed to be weak or very weak.
Next, we synthesize key findings (taking into account relative strengths and comparing only what is truly comparable) to produce a meta-synthesis that emphasizes convergent findings and notes disagreements. The result is a CHRSP meta-synthesis that is highly specific (i.e., compares apples to apples), takes into account the methodological strengths and weaknesses of the systematic review evidence, assesses the true size of the evidence base (i.e., the number of individual studies involved) and emphasizes convergent findings. Our knowledge users have indicated that this rating system makes intuitive sense to them and gives them confidence in the findings presented.
5. Contextualization: CHRSP helps provincial decision-makers in NL understand not only what works, but also what will work here, by focusing on likely effects and implementation issues.
"CHRSP helps provincial decision makers in NL understand not only what works, but also what will work here, by focusing on likely effects and implementation issues."
CHRSP assesses contextual implications for the feasibility, acceptability and health equity impacts of the studied intervention(s) to help decision-makers assess their suitability within local context(s). CHRSP interviews community and system stakeholders and reviews provincial data to uncover relevant contextual factors such as demographics, sites/design of service, health human resources, service organization and delivery, and political factors.
6. Interpretation: Key synthesis findings are considered together with contextualization factors to develop a summary of implications for decision-makers. By using the term “implications” (rather than “recommendations”), CHRSP acknowledges that research evidence is one of multiple inputs that health system decision-makers must consider.
7. Dissemination/ Evaluation: Once an external expert has reviewed the report, the final draft is reviewed by the team and our senior health system partners before dissemination. CHRSP hosts meetings/webinars for health system partners, academics and community/patient/caregiver stakeholders. Reports are published online and widely shared. CHRSP then hosts further meetings to optimize uptake. Once time has elapsed for consideration by decision-makers, CHRSP seeks stakeholder feedback on the usefulness/uptake of each report. CHRSP updates its knowledge syntheses every five years and advises our health system partners about any changes to the scientific evidence since the release of our initial reports.
Implementation
CHRSP started out by working with senior leaders (i.e., deputy ministers and regional health authority CEOs); focusing on these key relationships helped establish a solid foundation for the program. The ongoing commitment of these leaders is central to the program’s success.
Implementation challenges for the program have included the following:
- constraints on leaders’ time; in 2009, we introduced CHRSP champions, senior officials in each Regional Health Authority and government department who link CHRSP to other organizational decision-makers and to the leadership
- turnover of NLCAHR staff as a challenge to productivity
- turnover in partner organizations producing delays in topic selection and the need for regular orientation/training
- growing demand from the health system for more reports more quickly; in response, a computerized ERS and two shorter project formats were introduced—Rapid Evidence Reports and Jurisdictional Snapshots
- patient and informal caregiver perspectives were missing from our teams; in 2017, CHRSP introduced a Patient Caregiver Advisory Council to incorporate these important perspectives.
Evaluation and Impact
Decisions take time. CHRSP waits three years before surveying stakeholders about uptake of its reports. We email all participants on the original project teams and everyone invited to attend the dissemination of each report and we ask them the following questions:
- Was this report useful/relevant to your organization? If so, how?
- If the report was not useful or relevant, please tell us why not and how it might have been improved.
Feedback has been overwhelmingly positive. CHRSP reports have informed policy/practice directions on a variety of issues, including mobile mental health response, age-friendly acute care, youth residential treatment centres and options for rural dialysis. To access the feedback report, go to: http://www.nlcahr.mun.ca/CHRSP/CHRSP_FEEDBACK.pdf.
Lessons Learned
- It is crucial to build/maintain relationships with partners and to involve them fully in the process.
- “Pull” works better than “push”—studies proposed and prioritized by decision-makers get better uptake.
- Context matters—decision-makers prefer reports that address what will work here.
- Contextualization is complicated, but developing a template to structure contextualization interviews is helpful.
- Although developed for use in NL, CHRSP can be adapted for use in other jurisdictions with similar characteristics and needs.
CHRSP is currently developing a proposal to CIHR for adapting its approach to include two other provinces with significant rural populations.
Back to Top.
Testing integrated knowledge translation processes to improve the participation of children with disabilities in leisure activities in British Columbia
Ebele Mogo,1 Keiko Shikako-Thomas,1 Annette Majnemer,1 Jonathan Lai,1 Sheila Kennedy,2 Vivien Symington,3 Kellie Duckworth2
1McGill University, 2Sunny Hill Health Centre for Children, 3Club Aviva Recreation
Background and Rationale
About 4.6% of Canadian children and youth have an identified sensory, cognitive, physical or developmental disability.1 In British Columbia, about 15% of the population (over 500,000 people) have a disability.2 Research has found that participation in physical activity is related to improved mental health, alertness and resilience to the stresses of life.3 However, people with disabilities are more vulnerable to poor health outcomes4 and have poorer access to health education, health promoting activities and care.5 Therefore, it is crucial to improve policies to ensure their improved physical activity participation.
Objective(s)
Our overarching goal was to bridge the evidence-to-policy gap and advance the methods of integrated knowledge translation to inform policy-making. Specific goals included the following:
- Improve the methods for engaging community partners and decision-makers in discussions on solutions related to leisure promotion for children with disabilities.
- Tailor and convey research-based information as well as community stakeholders’ priorities to policy makers.
- Test the utility of a policy dialogue—a convening of policy decision-makers and community organization—in bridging research and policy.6
Initiative
The first step in this project involved convening a community forum where organizations were consulted to identify relevant frameworks on leisure promotion for children with disabilities. The National Framework for Recreation in Canada7 was identified as a key federal guideline with potential provincial reach but low application due to a lack of actionable items. We convened a structured meeting of these organizations to identify actionable points within this framework. Based on the top three identified priorities—inclusion, access and capacity building—we conducted a systematic rapid review of the literature on community-based and policy interventions promoting those constructs as outcomes.
We developed a targeted policy brief that took into account decision-makers’ and community organizations’ preferred formats (quantitative data or narrative data). The briefs were distributed to the 25 potential dialogue participants who were also identified by grassroots stakeholders (namely Club Aviva, Sport for Life, Sunny Hill Health Centre for Children and Child Health BC), and sampled purposefully to represent different levels of decision-making pertinent to leisure promotion for children with disabilities. Seventeen participants representing provincial, municipal and local programming levels participated in the policy dialogue. To access the evidence on promoting participation, go to: https://www.childhooddisability.ca/wp-content/uploads/2017/12/researchbrief_dec20.pdf.
Implementation
The research team presented the current research on children with disabilities and participation in leisure activities. The team also presented a solution previously chosen by stakeholders as a priority, namely the Jooay App,8 which lists adaptive and inclusive leisure activities across Canada. The research team emphasized the process through which the policy dialogue had been convened: through the research evidence on the priorities chosen by community organizations. Following this, the decision-makers and the community organizations present were invited to discuss the information in relation to their own future organizational and individual goals. They applied design-thinking and strategic planning tools to reflect on implementation considerations related to the policy recommendations from the policy brief.
Evaluation and Impact
Participants completed a structured evaluation of the policy dialogue and were invited to participate in a follow-up semi-structured interview to discuss their perspectives on the dialogue. Twelve participants were interviewed in the month following the dialogue. We used a survey and qualitative interviews to explore participants’ demographics and experiences with the dialogue. Ninety-three percent of participants had experience working with people with disabilities; 67% had a post-graduate degree and 33% of had a bachelor’s degree. Just over one-third of participants (34%) represented the provincial government, while other sectors represented included school boards, municipal governments and NGOs.
"Participants stated that the highest value they derived from the dialogue was the opportunity for future collaborations with participants and access to the policy brief as a reference tool for their ongoing work."
Participants indicated the following:
- They gained information to support ongoing projects and fuel discussions with colleagues.
- The dialogue was useful in helping them to learn about resources and to broaden their network.
- They were satisfied with the dialogue and their ability to contribute to it.
- The dialogue was a good use of their time and would make a difference in developing strategies to promote participation in leisure for children with disabilities.
- There was a perceived need to represent more diverse voices.
- The highest value they derived from the dialogue was the opportunity for future collaborations with participants and access to the policy brief as a reference tool for their ongoing work.
Lessons Learned
Strategies to inform policy-makers about evidence should include opportunities for engaging with a variety of stakeholders and integrating the context-specific information acquired from them. Through this process we learned that a common challenge among decision-makers is the training and capacity gap in gathering and applying research evidence. Other challenges include the lack of collaborative learning networks, which can be promoted through dialogues like the one we convened. In supporting leisure programs for children with disabilities, barriers are quite common and include financial constraints, negative attitudes or lack of knowledge/training of staff, poor customer satisfaction, language barriers, lack of access to adapted activities in regions outside of urban centres and difficulty in assembling a critical mass to initiate programs. We hope to build upon this study by exploring policy-makers’ perceptions of the content presented to them, assessing the long-term impact of policy content and organizing future dialogues across Canada based on our learnings from this process.
References
1 Bassett-Gunter, R.L., Ruscitti, R.J., Latimer-Cheung, A.E., & Fraser-Thomas, J.L. (2017). Targeted physical activity messages for parents of children with disabilities: A qualitative investigation of parents’ informational needs and preferences. Research in Developmental Disabilities, 64, 37-46.
2 Accessibility 2024 - Province of British Columbia. (2017). [ONLINE] www2.gov.bc.ca. Available at: https://www2.gov.bc.ca/gov/content/governments/about-the-bc-government/accessibility (accessed November 2017).
3 Street, G., James, R., & Cutt, H. (2007). The relationship between organised physical recreation and mental health. Health Promotion Journal of Australia, 18(3), 236-239.
4 Kuper, H., Smythe, T., & Duttine, A. (2018). Reflections on health promotion and disability in low and middle-income countries: Case study of parent-support programmes for children with Congenital Zika Syndrome. International Journal of Environmental Research, 15, 514.
5 Davis, K., Carter, S., Myers, E., & Rocca, N. (2018). Health promotion for young people with profound and multiple learning disabilities. Nursing Children and Young People, 30(01).
6 Shikako-Thomas, K., Majnemer, A., Mogo, E. M., Lai, J., & Kalaba, M. (N.D.). Childhood Disability Link. Promoting the participation of children with disabilities in leisure activities. Available at: https://www.childhooddisability.ca/wpcontent/uploads/2017/12/researchbrief_dec20.pdf.
7 The Framework for Recreation in Canada. (2018). Available at: https://www.cpra.ca/about-the-framework/.
8 Jooay.com. (2018). Connecting children and youth with disabilities to leisure. Available at: http://jooay.com.
Back to Top.
Building a cultural foundation for evidence-informed decision making: An evaluative thinking communications campaign
Background and Rationale
Evaluation is an important tool to support evidence-informed decision making (EIDM) in public health organizations. However, the capacity to do high-quality evaluation in small organizations is often lacking.
One factor that supports evaluation capacity is a learning organizational culture,1 which involves the investment in knowledge and learning for greater organizational innovation and adaptability.2 Through an evaluation capacity assessment as part of the Evaluation Capacity Building (ECB) Locally Driven Collaborative Project (LDCP),3 the Huron County Health Unit (HCHU) identified a need to build a learning organizational culture as a foundation for evaluation and EIDM.
"By encouraging more use of ET, staff could be empowered to identify assumptions, ask important questions, think about the evidence and make evidence-informed decisions in their daily work."
Staff have many competing priorities and limited time to participate in extra projects. Encouraging more evaluative thinking (ET)—critical thinking applied to evaluation, motivated by inquisitiveness and a belief in the value of evidence4—was identified as a way to begin to shift the organizational culture without additional workload for staff. By encouraging more use of ET, staff could be empowered to identify assumptions, ask important questions, think about the evidence and make evidence-informed decisions in their daily work.
Objectives
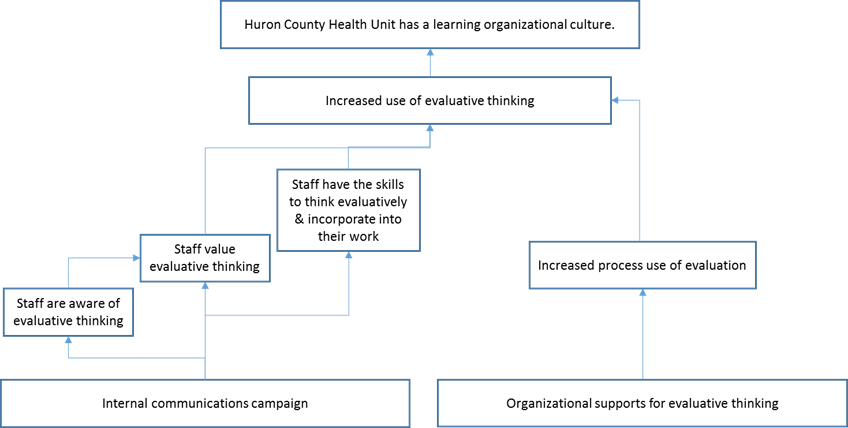
The goal of this initiative was to create a cultural foundation where evaluation and other forms of evidence are valued and used. The specific objectives of the internal campaign were to make staff more aware of ET, increase the value that staff place on ET and increase the skill that staff have to think evaluatively and incorporate ET into their work. The program logic for the ET strategy is described below.
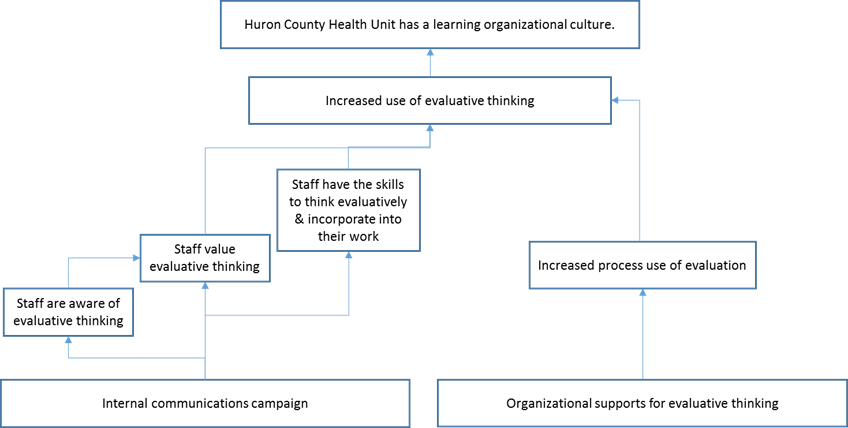
Initiative
Evidence from a variety of sources was incorporated into campaign planning. The local context was assessed through a survey of all staff to get a baseline of ET in the organization using the Evaluative Thinking Inventory (ETI).5 Literature on ECB was incorporated from the LDCP scoping review.6 The concept of ET was integrated into the campaign based on the work of Buckley and colleagues7 and was supplemented by initiatives found in grey literature. Since ET is a relatively new concept, the availability of peer-reviewed ET literature was limited. An internal advisory committee provided evidence on staff preferences. Data on staff communication preferences from previous evaluations of internal campaigns was also used. Resource availability limited the scope of the project to a four-week time frame, $300 budget and one staff lead.
The above evidence was integrated to develop a communications strategy with all HCHU staff as the target audience. This represented a diverse range of public health professionals, including health promoters, public health nurses, public health inspectors, managers and program support. The key messages of the campaign included the following:
- ET is critical, actionable and happens anytime.
- ET can help improve our programs, services and internal culture.
- It’s easy to add more ET into your everyday work.
The HCHU’s graphic designer developed a logo and branding, with the slogan “Think Evaluatively. Question. Assess. Improve.”

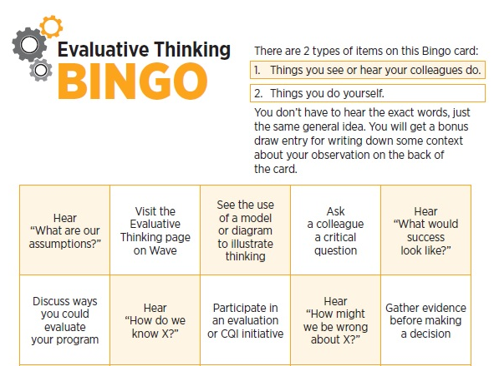
The campaign used multiple media and was conducted over four weeks. Components of the campaign included:
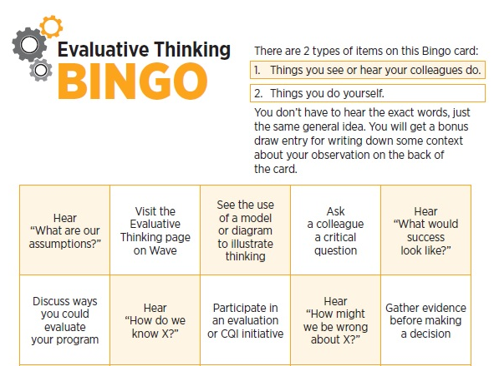
- Intranet content and blog posts
- Hour-long workshops (e.g., critical friend speed dating, six thinking hats)
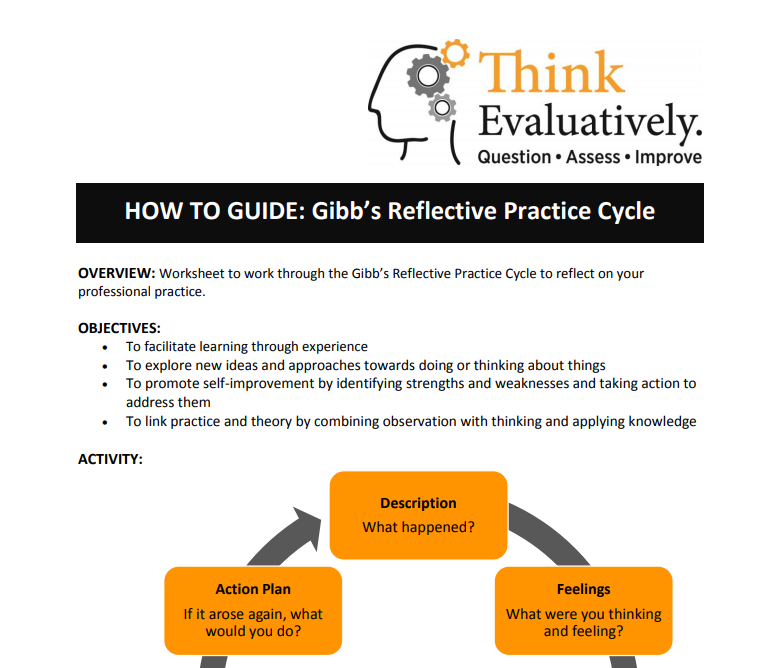
- Mini workshops (e.g., The Cookie Experiment, Gibbs reflective cycle, Paradigms exposed)
Each workshop was accompanied by a “how-to guide” so that staff could implement the workshop with their own teams or networks.
Implementation
Key factors to the success of the initiative were the recent introduction of an intranet, strong management support for the campaign and external support for the project through the ECB LDCP. The intranet provided a place to house and advertise campaign materials. Managers encouraged participation and allowed staff time to participate in workshops. The LDCP provided a framework and deadlines for the project.
After the initial 2016 ET campaign, the campaign was repeated in the fall of 2017, and there are plans for another iteration in 2018. Supporting a culture of evaluative thinking was identified as one of the strategic approaches in the 2017–2020 HCHU Strategic Plan, so this continues to be a priority for the organization.
Evaluation
The ETI was re-administered post-campaign to evaluate the impact of the campaign. Campaign reach was assessed using web analytics and participation rates. Managers were also interviewed to determine their impression of ET use among staff.
The reach of the campaign was good, with 94% of staff indicating they participated in the campaign. In an organization with 65 FTEs, there were 277 intranet site visits and 255 blog visits. Seventeen comments were added to blog posts, 27 staff participated in Bingo and 58 individuals participated in the interactive staff workshops. When asked, staff were able to recall the key messages of the campaign.
ETI results showed that the campaign successfully increased staff understanding of and their perception of the value of ET. The percentage of staff with at least a working knowledge of ET increased from 69% to 89% after the campaign. One of the ET dimensions with the greatest increase was “I seek evidence for claims and hypotheses.” Managers indicated they noticed that ET had become a new part of staff vocabulary.
Lessons Learned
There are barriers for staff to incorporate ET into their work, including high workloads and not understanding how it can apply to their role. This was a short four-week campaign, and continued effort will be needed to shift organizational culture, building toward a learning organization where EIDM is second nature.
If you are interested in any of the campaign materials described, please contact Kristin Beaton at kbeaton@huroncounty.ca.
References
1 Hotte, N., Simmons, L., Beaton, K., & the LDCP Workgroup. (2015). Scoping Review of Evaluation Capacity Building Strategies. Cornwall, Ontario, Canada.
2 Akhnif, E., Macq, J., Idrissi Fakhreddine, M.O., & Meessen, B. (2017) Scoping literature review on the Learning Organisation concept as applied to the health system. Health Research Policy and Systems, 15, 16.
3 Hotte, N., & the Building Evaluation Capacity in Ontario’s Public Health Units LDCP Workgroup. (2015). Evaluation Capacity Assessment Instrument. Cornwall, Ontario, Canada.
4 Buckley, J., Archibald, T., Hargraves, M., & Trochim, W.M. (2015). Defining and teaching evaluative thinking: Insights from research on critical thinking. American Journal of Evaluation, 36(3), 375-388.
5 Buckley, J., & Archibald, T. (2011). The Evaluative Thinking Inventory. Available at: http://comm.eval.org/HigherLogic/System/DownloadDocumentFile.ashx?DocumentFileKey=687883a4-0ef5-4312-9b15-8b67ed217434&forceDialog=0
6 Hotte, N., Simmons, L., Beaton, K., & the LDCP Workgroup. (2015). Scoping Review of Evaluation Capacity Building Strategies. Cornwall, Ontario, Canada.
7 Buckley, J., Archibald, T., Hargraves, M., & Trochim, W.M. (2015). Defining and teaching evaluative thinking: Insights from research on critical thinking. American Journal of Evaluation, 36(3), 375-388.
Back to Top.
Making evidence-informed decisions about the Alberta Public Health well-child visit: The art and the science
J.Cyne Johnston, Farah Bandali, Maureen Devolin, Scarlett Ngoka, Dolly Bondarianzadeh
Alberta Health Services
Background and Rationale
In Alberta, each child is eligible to receive well-child clinic (WCC) visits through their local Alberta Health Services’ (AHS) Public/Community Health Clinic. WCC visits include all publicly-funded childhood immunizations as well as a number of health assessment, promotion and education activities. Examples of some of these non-immunization activities include growth measurement, injury-prevention messaging and breastfeeding and nutrition support. The timing of the WCC visits is aligned with the provincial immunization schedule. Families attend clinic when their children are 2, 4, 6, 12 and 18 months of age, and before school entry at 4 to 6 years of age. In addition to the health assessments and immunization, WCC visits offer parents the opportunity to ask questions and make connections to other health and community services. In Alberta, 56,428 babies were born in 2015,1 resulting in approximately 282,390 WCC visits in 2015.
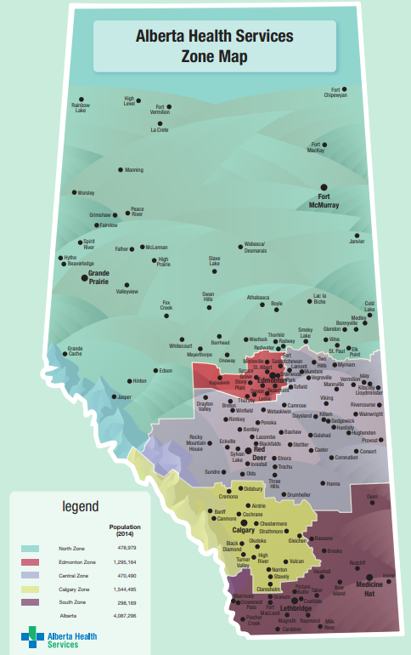
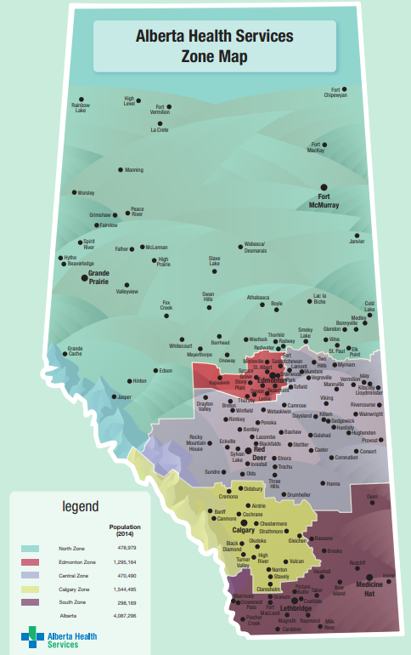
In recent years the province had increases in both the population and the number of immunizations provided during WCC visits, however the funding and time allocated for each visit has not increased. This led to a decline in the time available for non-immunization, health promotion activities. Concurrently, it was identified that there were regional differences in the activities offered to families across the province. While AHS has been the single healthcare provider in the province since 2009, there are still differences in the delivery of health services across the five regional zones. Each zone has geographical, cultural and demographic differences that influence their health service delivery.
Representatives from each zone joined the provincial health promotion team, decision-makers and researchers to decide which non-immunization activities should be consistently offered across the province, including which should be prioritized and which ones potentially discontinued. This group was highly motivated to make fiscally responsible, evidence-informed decisions about WCC service delivery.
Objective
The objective of this initiative was to examine and decide on the routine, non-immunization public health WCC activities to be completed across the province of Alberta.
Initiative
Stakeholders were engaged from the start to establish initiative goals and objectives. These stakeholders included regional front-line public health managers and operational directors, researchers in maternal-child health and health promotion experts. These same stakeholders were engaged throughout the process. Prior to collecting evidence, decision-making criteria and a ranking system were identified to help prioritize WCC non-immunization activities. Criteria considered important to decision-making included: literature-informed best practice, required organizational policies or directives for practice, potential for improving the health of the population, patient safety, parent priorities, evaluability, alignment with organizational priorities and feasibility. These criteria were further confirmed as being comprehensive after scanning other work within Alberta, other jurisdictions and the academic and grey literature.2
The collection of evidence
The decision-making criteria helped identify which types of evidence were needed to support decision-making and what project work needed to be undertaken.
An environmental scan was used to document current practices across the province. All WCC manuals and practice and support documents were requested and reviewed to identify current non-immunization activities and interventions across the regions (zones). Data were then validated through key informant interviews. It was essential to understand the details of each of the activities, in each region, in order to identify variations in practice and to collect adequate details about the intervention for the review of evidence that followed. An example of one identified activity that was common to all five zones was postpartum depression screening of new mothers using the Edinburgh Postpartum Depression Screening Tool. The scan identified variations in the cut-off scores used to identify mothers at risk as well as the well-child visit in which the screening occurred. In all, 19 different WCC activities were identified.
A rapid review of the literature was conducted for each of the WCC activities to determine if there was evidence of effectiveness to support the current clinical practices. Systematic reviews were primarily used, while clinical practice guidelines and individual research studies were used when systematic reviews were unavailable. Searches of the Cochrane Library were conducted first. Google Scholar, Cumulative Index to Nursing and Allied Health Library (CINAHL), PubMed and Medline were used if the searches of Cochrane were unsuccessful. No formal quality assessment was undertaken. The evidence review provided insight into which activities were effective and the details about best clinical practice.
Needs of parents were identified through a review of research literature, local evaluation/quality improvement data and national-level reports that examined parents’ primary concerns during infancy and early childhood. Parents’ priorities were ranked based on the most frequently occurring topics. Breastfeeding, sleep, injury prevention and maternal mood were some of parents’ key concerns.
A review of internal organizational policies, provincial directives and priorities was conducted by searching internal websites for relevant policies and priorities. Stakeholders were also asked to identify regional policies that determined practice requirements. The WCC activities that were dictated by policies and priorities were flagged. Four organizational policies were identified: postpartum depression screening, childhood growth measurement, safe infant sleep and tobacco and smoke-free environments.
The potential for improving the health of the population was assessed by reviewing the WCC activity-related data from population-level health status assessments. Evaluability was assessed by examining the capability of monitoring health outcomes of each WCC activity through existing data systems. Alberta Health Services stakeholders weighed in on patient safety and operational feasibility.
Ranking exercise
Once all of the evidence was gathered and synthesized, the decision-making criteria were revisited to assess how well each of the WCC activities “scored” on each of the criteria. Each stakeholder independently applied a three-point scale to each criteria, for each activity. The scores of each of the criteria were summed, resulting in a total score for each WCC activity for each stakeholder. WCC activities were then ranked from top to bottom for each stakeholder, based on total scores. Delphi analysis for consensus building (based on the median of total aggregated score of each activity) was used to determine the final ranking of activities.3 These ranking data were used to guide conversations and build consensus regarding which WCC activities should be prioritized or discontinued across the province.
Evaluation and Impact
Success of the project was gauged by continuous stakeholder participation and satisfaction. Consensus regarding which non-immunization activities should be consistently offered in public health WCC visits was achieved. The next steps will be the implementation and the evaluation of the standard activities across Alberta.
Lessons Learned
Many factors influence public health decision-making. Evidence from a variety of sources must be considered due to the multitude of factors that are involved in designing public health interventions. Additionally, the lack of certainty in public health literature and challenges in measuring health outcomes make decision-making both a science and an art.
"Additionally, the lack of certainty in public health literature and challenges in measuring health outcomes make decision-making both a science and an art."
One of the facilitators of this work was that AHS was formed over 10 years ago and has remained relatively stable for this period of time. Presumably, consensus building would have been more challenging if this had been in the early days of the formation of a single healthcare system. Due to this stability, the stakeholders were familiar with each other from work on other provincial policies and projects. A challenge of the project was bringing experts from different disciplines together to make decisions. Each brought a different perspective about the “most important factors” in decision-making. The a priori creation of criteria for decision-making, continuous stakeholder engagement and collection of evidence from a variety of sources aided the group in coming to consensus.
References
1 Government of Alberta. (2018). Interactive Health Data Application. Live Birth Data. Available at: http://www.ahw.gov.ab.ca/IHDA_Retrieval/selectCategory.do
2 Gray, M. (2009). Evidence-based healthcare and public health: How to make decisions about health services and public health (3rd ed.). Toronto: Churchill Livingstone.
3 Hsu, C.C., & Sandford, B.A. (2007). The Delphi technique: making sense of consensus. Practical Assessment, Research & Evaluation, 12(10).
Back to Top.
Appetite to Play: Healthy eating and physical activity in the early years
Sana Fakih,1 Jennifer McConnel-Nzunga,1,2 Jennifer Scarr, 1 PJ Naylor,2 Kristin McIlhenney,3 Alex Wilson,4 Vanessa Morley,5 Chris Wright,4 Nicole Fetterly5
1Child Health BC, 2University of Victoria, 3YMCA of Greater Vancouver, 4Sport for Life, 5Childhood Obesity Foundation
Background and Rationale
Birth to the age of 5 years is a time of rapid growth in children. Patterns and behaviours develop that will last into adulthood, directly affecting lifelong health and resilience.1 Healthy eating and physical activity are two behaviours that are essential to healthy child development. The Canada Food Guide recommends four servings of fruits and vegetables per day for children aged 2 to 3 years of age, and five servings for children aged 4 to 8 years.2 When it comes to physical activity, children between the ages of 1 and 4 years should be physically active 180 minutes per day, and for 3 to 4 year olds, 60 minutes of this should be energetic play.3 However, across Canada, less than 30% of children 4 to 8 years of age eat the recommended minimum number of servings of vegetables and fruits per day,4 and just 62% of 3 to 4 year olds are achieving the recommended activity levels for their age group.5 In addition, 76% of 3 to 4 year olds are engaging in more recreational screen time than is recommended by the Canadian 24-Hour Movement Guidelines,5 indicating sedentary behaviours are becoming more common in the early years.
Objective
Appetite to Play is a provincial intervention in British Columbia aimed at building the capacity of early years providers to promote and support healthy eating and physical activity in the early years (birth–5 years old).
"Appetite to Play is a provincial intervention in British Columbia aimed at building the capacity of early years providers to promote and support healthy eating and physical activity in the early years (birth-5 years old)."
Specifically, the initiative focuses on building food literacy and physical literacy skills in the early years. Food literacy is the knowledge, attitude and skills that people have about food. It is also about developing a positive relationship with food, finding the connection between cultural foods/traditional foods and well-being, and equipping children with the beginning skills to grow, select and cook food. The more children understand about food, the more likely they are to try new foods and eat a healthy diet. Physical literacy focuses on children having the fundamental movement skills and the motivation, confidence and competence to move for a lifetime. Skills such as hopping, running, jumping, throwing and catching are key building blocks for being physically active.
Initiative
Early years providers (e.g., those working in daycare centres, family-based daycares, preschools, parent participation programs or after-school daycare) have an important role in creating environments that support food literacy and physical literacy, considering that children spend about two-thirds of their waking hours (7 hours per day) in childcare.
Appetite to Play consists of five main components that early years providers have access to:
- An early years provider “toolkit” that includes an interactive website (www.appetitetoplay.com) with a variety of healthy eating and physical activity games, tips, ideas and recipes for early years providers to use in their settings. Early years providers are encouraged to share these resources with parents and families as well. The website, which is updated weekly, houses a set of interactive tools to assist early years providers in program planning (e.g., weekly meal and physical activity planners, self-assessments, etc.).
- A set of recommended practices on healthy eating and physical activity in the early years, developed by experts across the province, and linked to BC Child Care Licensing Regulations and DOLSOP Active Play and Safe Play Space standards.
- Food literacy and physical literacy training though in-person workshops and e-learning modules.
- Support and communication on a regular basis through social media, e-newsletters, webinars and mailouts.
- Networking opportunities through the development of a healthy eating and physical activity in the early years community of practice.
Appetite to Play incorporates best evidence in a variety of ways.
First, an extensive market research study was conducted with early years providers across British Columbia to understand current awareness and usage of healthy eating and physical activity resources; assess perceptions, attitudes and values regarding these resources; assess motivators and barriers to using the resources; and determine what information and resources are required by early years practitioners. This information was used to design the components, tools and delivery of the Appetite to Play initiative across BC. Early years providers also had input into the name of the initiative, as well as the marketing and branding material used to promote the initiative.
Second, the partner organizations in the initiative (Child Health BC, YMCA of Greater Vancouver, Childhood Obesity Foundation and Sport for Life) brought together subject-matter experts, who were identified through the Ministry of Health and BC health authorities, to develop and implement the healthy eating and physical activity best practice recommendations. These best practice recommendations were developed based on current evidence that the subject-matter experts brought forward and according to BC childcare licensing regulations. These subject-matter experts are also regularly contacted to provide feedback on website posts on physical activity and healthy eating in the early years to ensure that up-to-date and best practices are incorporated into the games, ideas, tips, recipes and other activities that are published on the website.
Third, a PhD trained evaluation coordinator was included as part of the project team to conduct an ongoing process evaluation that involved pre- and post-training surveys; qualitative interviews with early years providers, trainers and project stakeholders; web analytics; and training delivery feedback. The pre- and post-training surveys captured demographics, subject area knowledge and confidence, intention to change, assessment of resources and workshop satisfaction constructs, as well as facility policy and open-ended training experience questions. Review of this evidence allowed us to make “real-time” course corrections and improvements, such as website content improvement, changes to communication methods and adjustments to evaluation administration.
Implementation
Appetite to Play is funded by the BC Ministry of Health through a grant administered by the BC Alliance for Healthy Living Society. Grants were awarded to initiatives across the province that support the British Columbia Physical Activity Strategy, which is designed to guide and stimulate coordinated policies, practices and programs in physical activity that will improve the health and well-being of British Columbians, and the communities in which they live, learn, work and play.
Implementation of Appetite to Play is done through a coordinated partnership approach between four different organizations in British Columbia: Child Health BC (lead organization), the YMCA of Greater Vancouver, Childhood Obesity Foundation and Sport for Life. Each organization has a specific role and area of expertise in the partnership. Implementation is also supported through an advisory committee that was established during the early stages of the initiative. The advisory committee is comprised of leaders from early years organizations, health authorities and government ministries across the province. The members meet on a quarterly basis to provide guidance and strategy support for the implementation and promotion of Appetite to Play.
Training of early years providers across the province occurs through a “train the trainer” model. Three master trainers were trained in the content for the Appetite to Play in-person workshop, and they trained 75 regional trainers from various geographic communities across the province. The 75 regional trainers are responsible for delivering in-person workshops in their respective communities. In-person training in the communities for early years providers has been primarily hosted in partnership with BC’s Child Care Resource and Referral Centres (CCRRs). CCRR programs offer workshops and training to support quality child care and programming in the early years field in every community across BC. In-person training has also been supported through other childcare and early years programs such as Strong Start, the YMCA and municipal recreation.
An important part of implementing Appetite to Play is its communication and marketing activities. Postcards, brochures, branded giveaways and a promotional video have been created and used to promote Appetite to Play to early years providers across the province. Appetite to Play’s recommended practices are linked to childcare licensing regulations and standards of practice, and as such licensing officers promote the training and resources to early years providers as a tool that can be used to meet licensing requirements. Also, social media (e.g., Facebook, Twitter, Pinterest) and e-newsletters are used to promote the program.
Evaluation and Impact
Impact So Far
The initiative was launched in September 2017, and to June 2018 there have been 101 workshops delivered across the province and 1,226 early years providers trained.
Workshop participants are asked to complete a pre- and post-survey. Based on 662 pre- and post-workshop surveys completed, workshop participants were satisfied with the workshop content (97%) and delivery (96%), and considered the content of the in-person workshop to be new (73%) and useful (96%). Wilcoxon Signed Rank Tests (SPSS, v. 23) indicated that compared with the pre-survey, knowledge and confidence increased significantly for physical activity, physical literacy, healthy eating and food literacy after the in-person workshop (p<.001).
Most participants stated they had control over physical activity (80%) and healthy eating (70%) for children in their care, and were determined and motivated to promote physical activity (90% and 89% respectively) and healthy eating (87% and 89% respectively). Workshop participants also thought it was enjoyable to promote physical activity and physical literacy (91%), and intended to limit sedentary behaviours in their settings (85%). However, participants stated that promoting healthy eating (27%) and physical activity (22%) for the children in their care will be difficult for some.
Lessons Learned
A key element of the success of Appetite to Play was the considerable engagement of early years providers in the planning and designing of the initiative. Understanding the practice needs of early years providers ensured the designed initiative is relevant, helpful, accessible and acceptable to its intended audience.
Another key element of the success of Appetite to Play has been the collaboration of the four partner organizations. This has resulted in using the expertise in their respective fields to strengthen the initiative. Specifically, Child Health BC provides expertise on children’s health and development to improve the health status and health outcomes of BC’s children; the YMCA of Greater Vancouver provides expertise on the coordination of training across the province; Sport for Life provides expertise on physical literacy and physical activity in children and youth; and Childhood Obesity Foundation provides expertise on healthy eating and food literacy for children and youth. Further, having an advisory committee that provides guidance and support to the initiative has promoted its uptake across the province.
Finally, a tiered approach to the delivery of the in-person workshop was also important. The centralized team, mostly located in Vancouver and Victoria, does not understand the local circumstances and needs of all the communities in BC. Ensuring that trainers deliver the workshops in the communities in which they live, work and already have established relationships is important for the delivery and uptake of the resources.
References
1 Waldfogel, J. (2004). Social Mobility, Life Changes, and the Early Years, CASE Paper 88. London: London School of Economics.
2 Health Canada. (2016). Canada’s food guides. Available at: https://www.canada.ca/en/health-canada/services/canada-food-guides.html.
3 CSEP. (2017). Canadian 24-hour movement guidelines for the early years (0–4 years): An integration of physical activity, sedentary behavior and sleep. Available at: http://csepguidelines.ca/early-years-0-4/.
4 Statistics Canada. (2004). Nutrition: Findings from the Canadian Community Health Survey, Overview of Canadians’ Eating Habits. Health Statistics Division.
5 Participaction. (2018). The 2018 ParticipACTION report card on physical activity for children and youth. Available at: https://www.participaction.com/sites/default/files/downloads/the_participaction_report_card_on_physical_activity_for_children_and_youth_-_2018.pdf
Back to Top.
Active & Safe Central: Injury prevention for sport and recreational activity
Dr. Shelina Babul (Co-PI),1 Dr. Ian Pike (Co-PI),1 Dr. Amanda Black,2 Dr. Sarah Richmond,3 Kate Turcotte,1 Samantha Bruin1
1BC Injury Research and Prevention Unit; BC Children's Hopsital; University of British Columbia, 2University of Calgary, 3Public Health Ontario
Background and Rationale
Injuries related to sports and recreational activities have a substantial cost in terms of reduced productivity and impact on the healthcare system and overall quality of life. Despite the risks for injury, physical activity in the form of sport and recreation participation has substantial health benefits and should not be avoided. Physical activity is one of the recommended strategies for maintaining a healthy weight and the prevention of a number of health-related conditions including cardiovascular disease, diabetes and certain types of cancer. Although there are evidence-based interventions that support the reduction in injury risk across different sports,1,2,3 access to this information can be challenging, and guidance is often required to apply it appropriately.
Objective
Active & Safe Central addresses the need for easily accessible and translated evidence-based information to reduce the risk for sport and recreation-related injuries among children and youth ages 6 to 19 years and adults. The long-term outcomes of this initiative are expected to be a reduction in the number and rate of serious injuries related to sport and recreational activities.
"Active and Safe Central addresses the need for easily accessible and translated evidence-based information to reduce the risk for sport recreation-related injuries among children and youth ages 6 to 19 years and adults."
Initiative
Active and Safe Central is an online resource providing injury-prevention information for over 50 sports and recreational activities. The development of this resource involved a six-phase strategy informed by the project team members and key stakeholders, including SportMedBC, viaSport British Columbia, Parachute, the Sport Injury Prevention Research Centre, University of Calgary and BC Recreation and Parks Association. Active and Safe Central is led by BC Injury Research and Prevention Unit and funded by the Province of BC through a grant administered by the BC Alliance for Healthy Living. Grants were awarded to initiatives across the province that support the British Columbia Physical Activity Strategy, which is designed to guide and stimulate coordinated policies, practices and programs in physical activity that will improve the health and well-being of British Columbians, and the communities in which they live, learn, work and play.
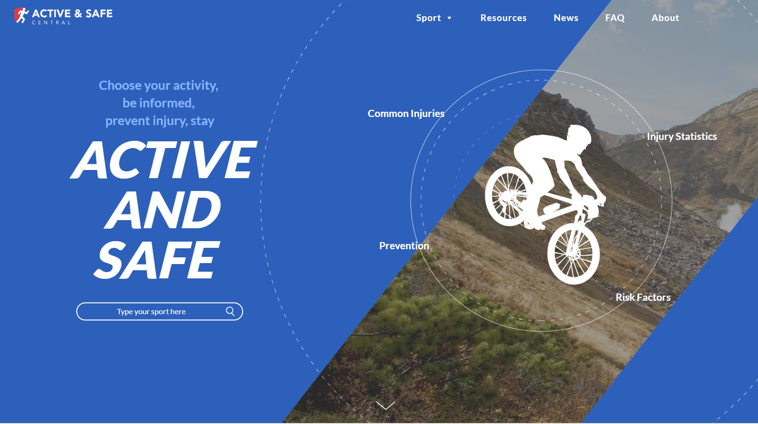
Phase 1: Prioritizing Sport and Recreational Activities and Recruitment for Conducting the Synthesis of Evidence
Over 60 sports and recreational activities were identified for inclusion in the Active & Safe Central resource. For the purposes of conducting the evidence reviews, the identified sports and recreational activities were grouped into categories based upon similar movement mechanisms (e.g., racquet sports). In addition, a preliminary search of each sport by outcome was conducted to assess the volume of literature.
Trainees from the Canadian Injury Prevention Trainee Network (http://ciptn.org/) completed evidence reviews and summary reports. This network was established in 2013, building upon the working model of the CIHR Team in Child & Youth Injury Prevention (2010–2016, http://childinjuryprevention.ca/). The network was formed to provide professional development and employment opportunities to graduate students with an interest in injury prevention. Under close supervision, 18 graduate students from across Canada worked independently or in pairs to develop search strategies in consultation with a university librarian and to review the evidence.
Phase 2: Completion of the Reviews and Summary Tools
An evidence synthesis framework was used for the collection and synthesis of injury-prevention evidence for all identified sports and recreational activities.4 The outcomes for the reviews included injury incidence, risk/protective factors, interventions and information on the implementation or evaluation of interventions.
Searches began using a hierarchy of evidence approach5 for all identified sports and recreation activities. Evidence summaries were searched to provide a comprehensive review of the incidence, risk and protective factors, and interventions to reduce the impact of injury. Where evidence summaries were not found, systematic reviews published within the past 10 years (2007–2017) were then searched by outcome. In the absence of a systematic review(s), or where reviews were published before 2007, primary studies were then searched by outcome.
In addition to reviews of published literature, researchers completed a search of relevant grey literature sites/organizations that publish best practice recommendations for injury prevention. Such organizations included injury-prevention organizations (e.g., Sport Injury Prevention Research Centre), health-related government sites (e.g., Public Health Agency of Canada), non-governmental organizations (e.g., Parachute) and sport-specific organizations (e.g., Hockey Canada).
Data from identified studies were extracted and critically appraised using the following tools, as appropriate:
- Health Evidence Quality Appraisal Tool6 (systematic reviews—risk factor and intervention studies)
- Downs and Black Critical Appraisal Tool7 (primary studies)
- MORE Tool8 (systematic reviews and primary studies— incidence/prevalence studies)
For each sport and recreational activity, researchers integrated information from the review into an evidence synthesis tool as well as a summary report. Due to gaps in the literature for certain sports and recreation activities, a total of 51 sport-specific evidence synthesis tools and summary reports were completed and shared with experts to identify potential gaps in the synthesized evidence.
Excerpt from Soccer Evidence Review (https://activesafe.ca/wp-content/uploads/2018/04/Soccer_Final.pdf):
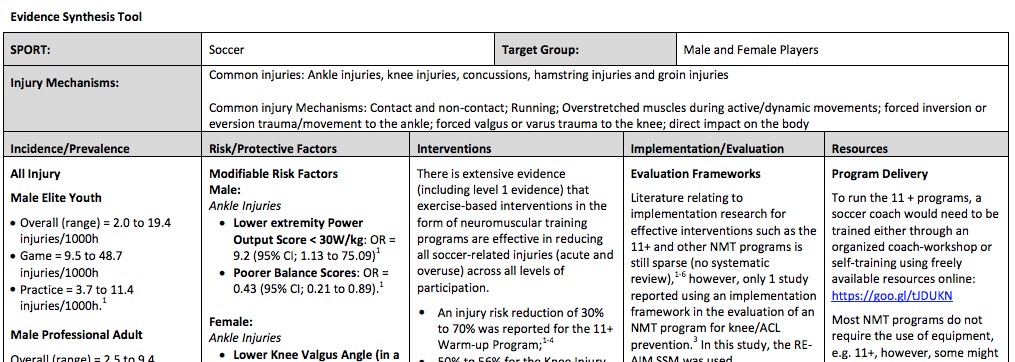
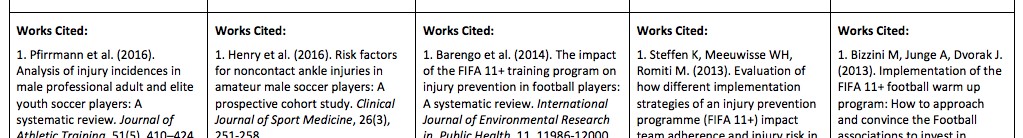
Phase 3: Knowledge Transfer Strategy and Digital Marketing Plan
Content and target audiences for the Active & Safe Central resource were determined based on the evidence reviews and summary reports. A digital marketing plan was developed to include social media, a media release and other messaging.
Phase 4: Scoping Document for the Central Online Resource
A scoping document outlining the content and delivery strategy for Active & Safe Central was developed, describing the organization and providing a detailed outline of the digital sports and recreation activities content pages. This vision was refined during the digital translation design process, guided by input from focus group participants including student athletes, parents, provincial sports organizations and injury-prevention stakeholders and researchers.
Phase 5: Content for Training Modules for Target Audiences
Goals of the Active & Safe Central resource included increasing users’ access to evidence-based sport and recreation injury information and supporting the implementation of injury-prevention strategies. Rather than duplicate the efforts of other sport injury groups, Active & Safe Central provides links to available evidence-informed injury-prevention digital material, including the following:
- Neuromuscular training modules for the prevention of sport injury in basketball physical education contexts developed by the Sport Injury Prevention Research Centre at the University of Calgary
- The Get Set training app from the International Olympic Committee (Apple | Android)
- The Fit to Play resource by the Oslo Sport Trauma Research Center
- The 11+ Warm-up
Phase 6: Development of Active & Safe Central Resources, Launch and Evaluation
Content from the evidence reviews was translated into clear messaging for use in a digital format. This included information on injury incidence, common areas of the body that are injured, risk factors for injury and prevention strategies, as well as any information gathered on the implementation or evaluation of prevention strategies. Digital sport and recreation content pages were populated with sport- and recreation activity-specific injury-prevention information together with visually engaging messages that were customized for participants and parents, coaches and teachers, officials and administrators, and health professionals.
In the prevention section of the resource, sport- and recreation activity-specific evidence-based prevention strategies are provided; however, for some sports and recreation activities, there was limited evidence supporting specific programs to prevent injury. In these cases, recommendations for the prevention of injury were made based on activities that have similar movement mechanics and patterns, or those that have similar types of injury. In addition, an “Other Considerations” section was developed to include useful information found in the grey literature search. This information, although not found in the research literature, was supported by experts in each sport or activity (e.g., local organizations, health experts).
Dissemination of the Resource
Active & Safe Central was launched at activesafe.ca on May 10, 2018 in alignment with International Move for Health Day. A media release was distributed through the research institute of BC Children’s Hospital and links were shared through social media and the BC Injury Research and Prevention Unit website and newsletter (www.injuryresearch.bc.ca). The project partners also disseminated the resource to their networks throughout Canada.
Evaluation, Impact and Ongoing Efforts
The media release resulted in 10 news articles by news outlets across British Columbia. Facebook ads promoting the tool and the online evaluation generated over 300 visits to the resource during a seven-day period post-launch. Initial post-launch results suggest that Active & Safe Central is a useful resource for providing Canadians with injury-prevention information for sport and recreation activities. During the first 40 days after launch, there were 2,306 visits to the Active & Safe Central website 6,340 pages were viewed and 87 people participated in an evaluation of the site. Overall, 94% of respondents agreed that Active & Safe Central is a helpful resource, 90% agreed that they learned something new and 90% agreed that the website is easy to use. Furthermore, 87% of respondents agreed that they will use the recommended injury-prevention strategies, 86% plan to share what they learned with others and 94% agreed that they would recommend this website to others.
Ongoing work on Active & Safe Central includes continued promotion of the resource by the BC Injury Research and Prevention Unit using social media, conference presentations, the development of informative prevention resource videos (e.g., physical literacy, training load, neuromuscular training and sleep hygiene) and manuscript development. Emerging sports and recreational injury-prevention evidence will be reviewed twice a year, and the resource will be updated as new information becomes available.
Lessons Learned
The most challenging aspect in the development of Active & Safe Central was the work required to concurrently conduct evidence reviews on an extensive number of sports and recreational activities. This challenge was met by grouping like activities together, assigning topics based on the amount of literature retrieved from preliminary searches and partnering with the Canadian Injury Prevention Trainee Network. The lesson learned is that the Canadian Injury Prevention Trainee Network is capable of conducting multiple related evidence reviews concurrently and efficiently, and this partnership was crucial to the success of the project.
References
1 MacKay, M., Scanlan, A., Olsen, L., Reid, D., Clark, M., McKim, K., & Raina, P. (2004). Looking for the evidence: a systematic review of prevention strategies addressing sport and recreational injury among children and youth. Journal of Science and Medicine in Sport, 7(1), 58-73.
2 Emery, C.A., Cassidy, J.D., Klassen, T.P., Rosychuk, R.J., & Rowe, B.H. (2005). Effectiveness of a home-based balance-training program in reducing sports-related injuries among healthy adolescents: a cluster randomized controlled trial. Canadian Medical Association Journal, 172(6), 749-754.
3 Emery, C.A., Roy, T.O., Whittaker, J.L., Nettel-Aguirre, A., & Van Mechelen, W. (2015). Neuromuscular training injury prevention strategies in youth sport: a systematic review and meta-analysis. British Journal of Sports Medicine, 49(13), 865-870.
4 Chambers, A., Richmond, S.A., Logan, L., Macarthur, C., & Mustard, C.A. (2014). The development of a framework to integrate evidence into a national injury prevention strategy. Journal of Public Health, 37(4), 671-677.
5 National Collaborating Centre for Methods and Tools. (2014). Evidence-Informed Public Health. Search: Efficiently search for research evidence. Available at: http://www.nccmt.ca/eiph/search-eng.html
6 Health Evidence. (2018). Quality Assessment Tool – Review Articles. Available at: https://www.healthevidence.org/documents/our-appraisal-tools/quality-assessment-tool-dictionary-en.pdf
7 Downs, S.H., & Black, N. (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology & Community Health, 52(6), 377-384.
8 Shamliyan, T., Kane, R.L., & Dickinson, S. (2010). A systematic review of tools used to assess the quality of observational studies that examine incidence or prevalence and risk factors for diseases. Journal of Clinical Epidemiology, 63(10), 1061-1070.
Back to Top.