January 2015 · Issue 113
In this issue:
- A closer look at NCCMTs video series: Understanding Research Evidence
- New from Public Health+
- Register now for week-long Evidence-Informed Decision Making workshop
- Congratulations!
- SAVE THE DATE!
A closer look at NCCMTs video series: Understanding Research Evidence
Remember, we created these short videos to explain some important terms that you may encounter in research evidence. They provide a valuable refresher or useful introduction to terms public health professionals need to make good decisions using research evidence.
This week: Understanding what a P value tells us
Many people know what a P value is, but struggle to explain it to someone else. And that’s exactly what you might need to do if you find yourself having to explain to community partners and clients why certain program decisions were made. Being able to explain in simple terms what a P value is and means may come in handy.
A P value reported in a study tells how likely it is that the reported result is true and is not a coincidence.
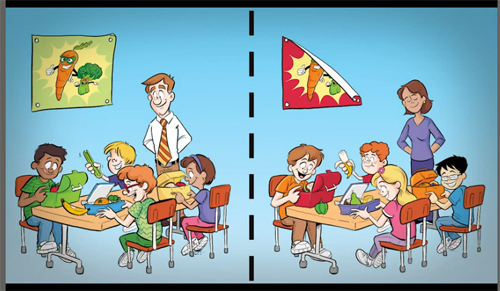
Using a hypothetical study on an intervention to promote healthy eating among children, Understanding what a P value tells us looks at what the reported P value tells us, and what it doesn’t tell us.
With practice, you will be able to use P values to help inform your public health practice decisions.
About the series
The Understanding Research Evidence series now includes ten short videos which explain key statistical terms: odds ratios, relative risk, confidence intervals, forest plots, clinical significance, types of reviews, and number needed to treat. The videos explain each term in plain language using realistic public health examples and engaging visuals.
Watch all the videos in the series!
The videos are available on YouTube and on the NCCMT website (http://www.nccmt.ca/resources/multimedia-eng.html). They are part of a series of products and services on the website and in the Learning Centre (http://www.nccmt.ca/learningcentre/index.php#main.html) designed to help you make good public health decisions, based on the best research evidence available.
New from Public Health+
Physical activity and cardiovascular risk factors in children: meta-analysis of randomized clinical trials.
OBJECTIVE: To assess the effects of physical activity interventions in preventing cardiovascular risk factors in childhood through a systematic review and meta-analysis of randomized clinical trials (RCTs). METHODS: A search of online databases (PubMed, EMBASE and Cochrane CENTRAL) was conducted from inception until June 2013. RCTs enrolling children 6-12years old conducted physical activity interventions longer than 6months, assessing their effect on body mass index (BMI), systolic (SBP) and diastolic blood pressure (DBP), total cholesterol (TC) and triglycerides (TG) were included. Data analysis was performed using a random-effects model. RESULTS: Of 23.091 articles retrieved, 11 RCTs (10.748 subjects) were included. Physical activity interventions were not associated with reductions of BMI [-0.03kg/m2 (95%CI -0.16, 0.13) I2 0%]. However, there was an association between the interventions and reduction of SBP [-1.25mmHg (95%CI -2.47, -0.02) I2 0%], DBP [-1.34mmHg (95%CI -2.57, -0.11) I2 43%] and TG [-0.09mmol/L (95%CI -0.14, -0.04) I2 0%], and increase of TC [0.14mmol/L (95%CI 0.01, 0.27) I2 0%]. CONCLUSION: As physical activity intervention programs lasting longer than 6months are associated with reductions in blood pressure levels and triglycerides, they should be considered to be included in prevention programs for cardiovascular diseases in schoolchildren.
The full text may be available from PubMed
Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or Plasmodium vivax malaria in endemic countries.
BACKGROUND: In settings where both Plasmodium vivax and Plasmodium falciparum infection cause malaria, rapid diagnostic tests (RDTs) need to distinguish which species is causing the patients` symptoms, as different treatments are required. Older RDTs incorporated two test lines to distinguish malaria due to P. falciparum, from malaria due to any other Plasmodium species (non-falciparum). These RDTs can be classified according to which antibodies they use: Type 2 RDTs use HRP-2 (for P. falciparum) and aldolase (all species); Type 3 RDTs use HRP-2 (for P. falciparum) and pLDH (all species); Type 4 use pLDH (fromP. falciparum) and pLDH (all species).More recently, RDTs have been developed to distinguish P. vivax parasitaemia by utilizing a pLDH antibody specific to P. vivax. OBJECTIVES: To assess the diagnostic accuracy of RDTs for detecting non-falciparum or P. vivax parasitaemia in people living in malaria-endemic areas who present to ambulatory healthcare facilities with symptoms suggestive of malaria, and to identify which types and brands of commercial test best detect non-falciparum and P. vivax malaria. SEARCH METHODS: We undertook a comprehensive search of the following databases up to 31 December 2013: Cochrane Infectious Diseases Group Specialized Register; MEDLINE; EMBASE; MEDION; Science Citation Index; Web of Knowledge; African Index Medicus; LILACS; and IndMED. SELECTION CRITERIA: Studies comparing RDTs with a reference standard (microscopy or polymerase chain reaction) in blood samples from a random or consecutive series of patients attending ambulatory health facilities with symptoms suggestive of malaria in non-falciparum endemic areas. DATA COLLECTION AND ANALYSIS: For each study, two review authors independently extracted a standard set of data using a tailored data extraction form. We grouped comparisons by type of RDT (defined by the combinations of antibodies used), and combined in meta-analysis where appropriate. Average sensitivities and specificities are presented alongside 95% confidence intervals (95% CI). MAIN RESULTS: We included 47 studies enrolling 22,862 participants. Patient characteristics, sampling methods and reference standard methods were poorly reported in most studies. RDTs detecting `non-falciparum` parasitaemiaEleven studies evaluated Type 2 tests compared with microscopy, 25 evaluated Type 3 tests, and 11 evaluated Type 4 tests. In meta-analyses, average sensitivities and specificities were 78% (95% CI 73% to 82%) and 99% (95% CI 97% to 99%) for Type 2 tests, 78% (95% CI 69% to 84%) and 99% (95% CI 98% to 99%) for Type 3 tests, and 89% (95% CI 79% to 95%) and 98% (95% CI 97% to 99%) for Type 4 tests, respectively. Type 4 tests were more sensitive than both Type 2 (P = 0.01) and Type 3 tests (P = 0.03).Five studies compared Type 3 tests with PCR; in meta-analysis, the average sensitivity and specificity were 81% (95% CI 72% to 88%) and 99% (95% CI 97% to 99%) respectively. RDTs detecting P.vivax parasitaemiaEight studies compared pLDH tests to microscopy; the average sensitivity and specificity were 95% (95% CI 86% to 99%) and 99% (95% CI 99% to 100%), respectively. AUTHORS` CONCLUSIONS: RDTs designed to detect P. vivax specifically, whether alone or as part of a mixed infection, appear to be more accurate than older tests designed to distinguish P. falciparum malaria from non-falciparum malaria. Compared to microscopy, these tests fail to detect around 5% ofP. vivax cases. This Cochrane Review, in combination with other published information about in vitro test performance and stability in the field, can assist policy-makers to choose between the available RDTs.
The full text may be available from PubMed
Register now for week-long Evidence-Informed Decision Making workshop
May 4 – May 8, 2015
Canadian Centre for Evidence-Based Nursing
McMaster University, Hamilton, ON
- Search for, access, and critically appraise the relevance and quality of evidence.
- Interpret and apply the evidence.
- Identify strategies to implement evidence-informed decision making (EIDM).
This workshop is open to participants of all skill levels related to EIDM. Health professionals, administrators, librarians, managers, policy makers, and faculty members are welcome to attend.
Visit http://www.ccebn.ca or contact Jennifer Yost at ccebn@mcmaster.ca to register.
Congratulations!
NCCMT is proud to announce that Alba DiCenso, professor emerita of McMaster's School of Nursing and the Department of Clinical Epidemiology and Biostatistics, will receive the Order of Canada for her research in evidence-based nursing and her contributions to the development of nurse practitioners.
The Order of Canada was established in 1967 to recognize outstanding achievement, dedication to the community and service to the nation. It recognizes people in all sectors of Canadian society for their varied contributions that have enriched the lives of others and made a difference to the country.
Alba DiCenso has provided exemplary leadership throughout her career with a focus on improving the health care of Canadians. She is internationally celebrated for advancing evidence-based nursing, and achieving full integration of nurse practitioners in and beyond Canada.
SAVE THE DATE!
February Spotlight on KT Methods & Tools webinar
Date: February 25, 2015 (1 PM, ET)
Tool Featured: Ontario Public Health Standards (OPHS) Evidence-Informed Planning Cycle
This toolkit can be used to inform program decisions through assessment, program development, implementation and evaluation. It is designed to match the specifications set by the Ontario Public Health Standards.